This is the story of Nayan (not his real name), a Bangladeshi construction worker, who was denied medical certificates despite suffering a serious work injury.
While at work on a fateful day in February 2023, a 500kg roof frame hanging from a crane swung and hit Nayan’s foot, causing his left ankle to swell with acute pain. Over the following two days, Nayan’s employer took him to three private clinics, each confirming the same diagnosis: left ankle fracture.
Then the employer brought Nayan to a fourth private clinic in Orchard – it was now two days after the accident – accompanied by the company’s supervisor and manager, where he had surgery to realign his broken bones and secure them with metal plates and screws. Over the following three months, Nayan returned to the same clinic six times for post-surgery appointments. He recalls that every time he asked the doctor for medical leave (what is colloquially referred to in Singapore as “medical certificate” or “MC”), the doctor would respond that he would consult Nayan’s employer.
Three months after the accident, Nayan’s ankle was healing well, but his mind was preoccupied with worry: he had not received any MC from any of the four clinics he had visited. This was when he decided to contact TWC2 for advice.
MCs are especially important in work injury cases. Under the Work Injury Compensation Act, an injured worker who is issued an MC for a workplace injury is legally entitled to compensation for lost income (also known as “MC wages”) for up to 1 year. In other words, MCs are a lifeline for them and their families. Given that Nayan’s injury was serious and would require a lengthy recovery period, his concerns about not having received any MCs were entirely justifiable.

Upon hearing his story, we advised Nayan to visit the A&E at a government hospital. Since all four clinics were chosen by his employer, and none had issued him any MCs despite it being obvious that he should have received them since he was clearly not able to work, we were concerned that something was amiss. We explained that visiting a government hospital, where his employer would have no influence, would be in his best interest. Within a few days, our volunteer accompanied Nayan, who was still on crutches, to a government hospital where he was given an appointment to see a specialist and, of course, an MC.
Next, with Nayan’s consent, we attempted to contact the four clinics on his behalf. In our experience with work injury cases, it is not uncommon for doctors to pass MCs directly to employers, especially when the clinics are so-called “company clinics”. If the clinics had done so, the injured worker might remain unaware that medical leave had been ordered. This turned out to be the case for the third clinic, which quickly provided a copy of a 3-day MC issued for Nayan. The first clinic openly admitted that they did not issue an MC because Nayan’s employer told him it was unnecessary, as they were taking him to see another doctor. The second clinic did not respond to our email.
The fourth clinic was a private clinic (“Clinic A”), located at Mount Elizabeth Medical Centre in Orchard. Including the date of surgery, Nayan had been treated by this Clinic A six times without seeing any MC. (At the seventh visit, Nayan successfully obtained an MC after showing a memo prepared by our caseworker, explicitly requesting an MC.) As Clinic A was unwilling to address our inquiry by email, a TWC2 volunteer accompanied Nayan to his eighth visit. During the consultation, in responding to the volunteer’s query about MC, the doctor confirmed that he had not previously issued any MCs, but agreed to issue six backdated MCs for the first six consultations and an additional MC for the eighth visit. This time, the doctor did not mention the need to consult with Nayan’s employer.
Nayan was relieved to finally receive MCs covering the past three months during which he had been unable to work. These MCs would eventually lead to MC wage payouts, allowing him to support himself and his family in Bangladesh. However, we noticed something unusual: the six MCs not only covered retrospective dates (starting from the date of surgery), but their issue dates were also back-dated, making it appear as though they had been issued at the time of each clinic visit. This raised a question: had the doctor issued these MCs earlier but failed to give them to Nayan? A closer examination ruled that out, as the MC numbers were sequential, indicating they were all issued at once rather than on separate occasions.
Back-dating the issue date of MCs is prohibited under the Ethical Code and Guidelines for Medical Practitioners issued by the Singapore Medical Council. While it is possible that this back-dating was due to an administrative oversight, it nonetheless raises concern that there may have been a deliberate attempt to conceal the doctor’s failure to issue the MCs at the time of consultation.
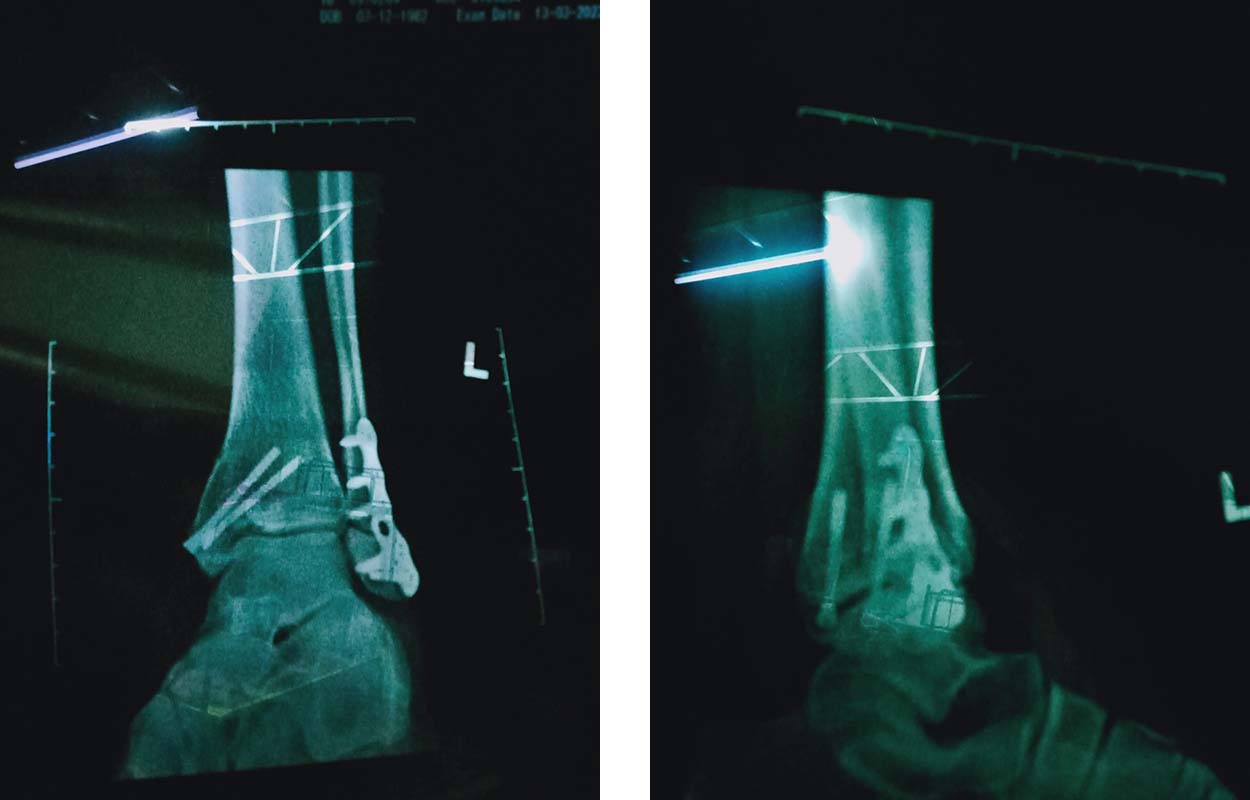
Unsurprisingly, that visit turned out to be Nayan’s last at Clinic A. Having lost trust in Clinic A over the MC ordeal, he chose to continue his treatment at the government hospital instead. This decision displeased his employer, and Nayan had to evade several attempts by them to bring him back to Clinic A. Fast forward 18 months, after undergoing a second surgery at the government hospital, Nayan received compensation for permanent incapacity and was finally able to return home to reunite with his family.
Employer influence on the issuance of MCs
Let’s reflect on Nayan’s experience. When a migrant worker suffers a work injury and seeks medical attention, it is common for a company representative to accompany him. Nayan was no exception. This practice can be understandable and, in some cases, even beneficial. Many low-wage migrant workers lack financial resources, family support, or sufficient English proficiency to communicate effectively with doctors. A responsible employer may therefore feel obliged to accompany the worker to ensure that treatment proceeds smoothly.
However, in the context of a work injury, the employer is also a party with a vested interest — and a potential conflict of interest can arise. Many workers have reported, and NGOs like TWC2 have directly observed, instances where employers attempted to downplay or conceal the seriousness of injuries. In some cases, employer representatives, often supervisors or managers, have tried to persuade the doctors not to issue an MC, even when the worker was clearly unfit for work.
This problem is not new. The Ethical Code and Guidelines for Medical Practitioners issued by the Singapore Medical Council (SMC) clearly stipulates that a doctor’s decision on whether to issue an MC must be based solely on medical grounds regardless of what patient’s employer prefers:
“B4(1) Medical certificates must be issued to patients only on proper medical grounds arrived at through good clinical assessment. You must not take into consideration extraneous factors such as who pays for the consultation, what benefits the patients may receive or what employers’ preferences may be.” (Emphasis added)
In 2019, a doctor was convicted of professional misconduct by a Court after failing to issue adequate medical leave to a migrant worker who had multiple work injuries, including broken ribs and a collarbone. This was said to be a case where an employer pressured doctors to issue no more than 2 days’ MC to avoid having to report the work accident to the Ministry of Manpower. Although the issue was partially addressed and the law was amended in 2020 to require employers to report any instances of MC or light duty, the tendency to hide or minimise MCs still persists.
The issue becomes more complex when the injured worker, the patient, declines or refuses an MC. Some doctors have justified the absence of an MC by claiming they are not obliged to issue one unless the patient requests it. While this may be acceptable for minor illnesses or for individuals who do not need to submit MCs to a third party, it cannot apply in the context of work injuries. In such cases, an MC carries direct implications for the worker’s legal entitlements to compensation, rest, and protection under the Work Injury Compensation Act.
When a worker rejects an MC, the reasons often stem from fear of employer retaliation or misplaced loyalty to the employer, who may wish to avoid reporting the incident to MOM. In these situations, we hope that the doctor should still prepare and keep the MC on file, so that a copy can be made available later if the worker changes his mind or gains a better understanding of its importance. The worker should also be informed that an MC has been prepared and is available for collection, ensuring that he is aware of the option.
Ultimately, the issuance of MCs in work injury cases is not merely a medical formality but a matter of safeguarding the worker’s rights. When employers interfere with medical decisions, or when workers feel pressured to reject the MCs they are entitled to, the integrity of the entire work injury compensation system is compromised. Ensuring that doctors act independently, that workers understand their rights, and that MCs are issued based solely on clinical judgment are paramount steps toward safeguarding injured workers’ access to fair compensation under the Work Injury Compensation Act.
TWC2 helped Nayan file a complaint about this doctor to the Singapore Medical Council. The complaint was attended to (it took about a year) but because the outcome was marked as confidential, we cannot write about it. That said, it’s quite fair to ask why it has to be confidential: whose interest is served by such a policy?
14203
